Bibigul Omirbayeva,
Chief Expert,
Department of Economic Policy Analysis
KazISS under the President of the Republic of Kazakhstan
In the global policy agenda, healthcare is increasingly regarded as a factor of national competitiveness. Nowadays, when countries strive to ensure the sustainability of their economies, human capital, and social systems, the primary healthcare (PHC) level plays a crucial role.
The accessibility of medical care, public trust, and the system’s ability to effectively respond to challenges, from chronic diseases to epidemics, are shaped at the level of clinics and family doctors, i.e., primary health care (PHC).
Analysis of the dynamics and structure of primary healthcare financing is becoming not only an industry-specific issue, but also a strategic one that directly affects quality of life, economic productivity, and fiscal sustainability.
Macroeconomic Context: Growth in Expenditure Amid Changes in its Structure
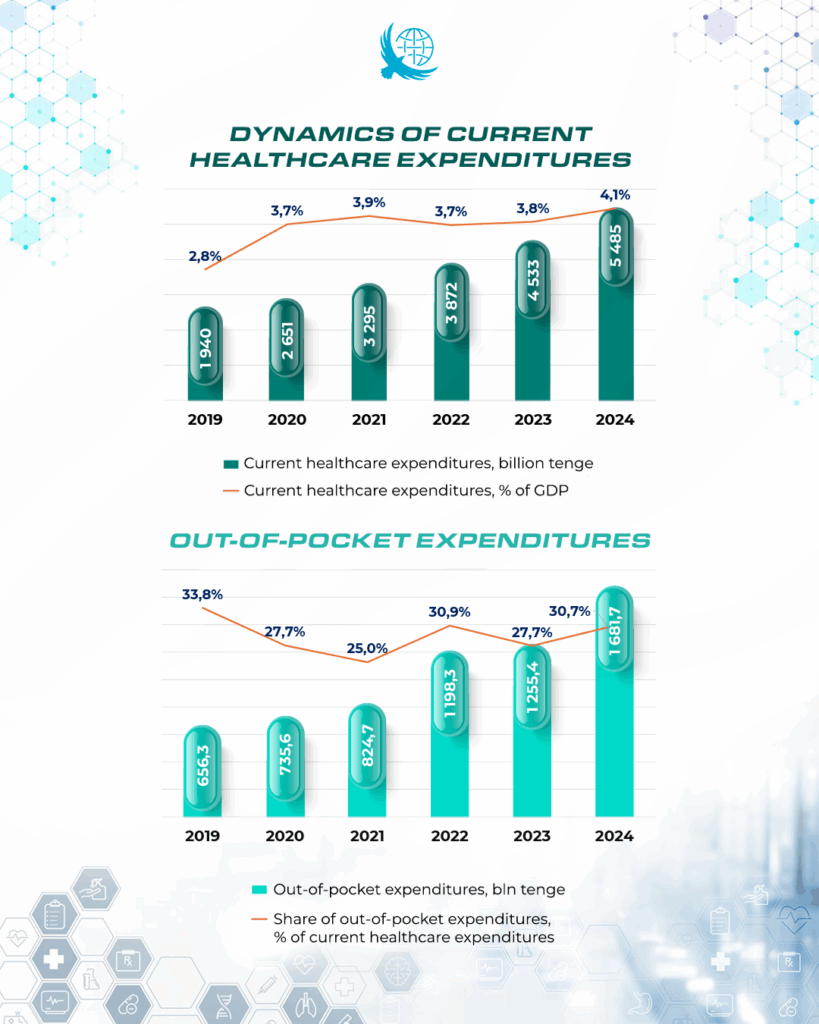
Between 2019 and 2024, current healthcare expenditures in Kazakhstan nearly tripled from 1.9 to over 5 trillion tenge demonstrating the sector’s priority status.
However, the structure of financing raises concerns:
- The share of government spending decreased by more than 6 percentage points (from 66% in 2023 to 59.2% in 2024);
- Out-of-pocket household expenditures reached 30.7% in 2024 (compared to 27.7% in 2023), exceeding the internationally recommended threshold for financial protection (20%).
The growth of out-of-pocket expenses indicates increasing financial pressure on households and the risk of reduced access to medical services.
PHC in Kazakhstan: Financing Principles and Practical Constraints
Primary healthcare in Kazakhstan is financed through a capitation principle, one of the most rational approaches globally. It allocates funds per enrolled patient, taking into account age, gender, and other risk factors.
This model is designed to promote efficient use of resources and control over service volumes. However, in practice, the per capita rate remains insufficient to cover all essential PHC functions, implement modern preventive programs, and retain qualified personnel at the primary level.
Financing PHC: Growth Without Prioritization of Prevention
Analysis shows that spending on primary healthcare increased from 1.1 to 2.8 trillion tenge over five years. However, the share of PHC in total healthcare expenditures remains stable or even declines. In other words, the increase in funding has been proportional to the general rise in healthcare spending, rather than reflecting a targeted strengthening of PHC priorities.
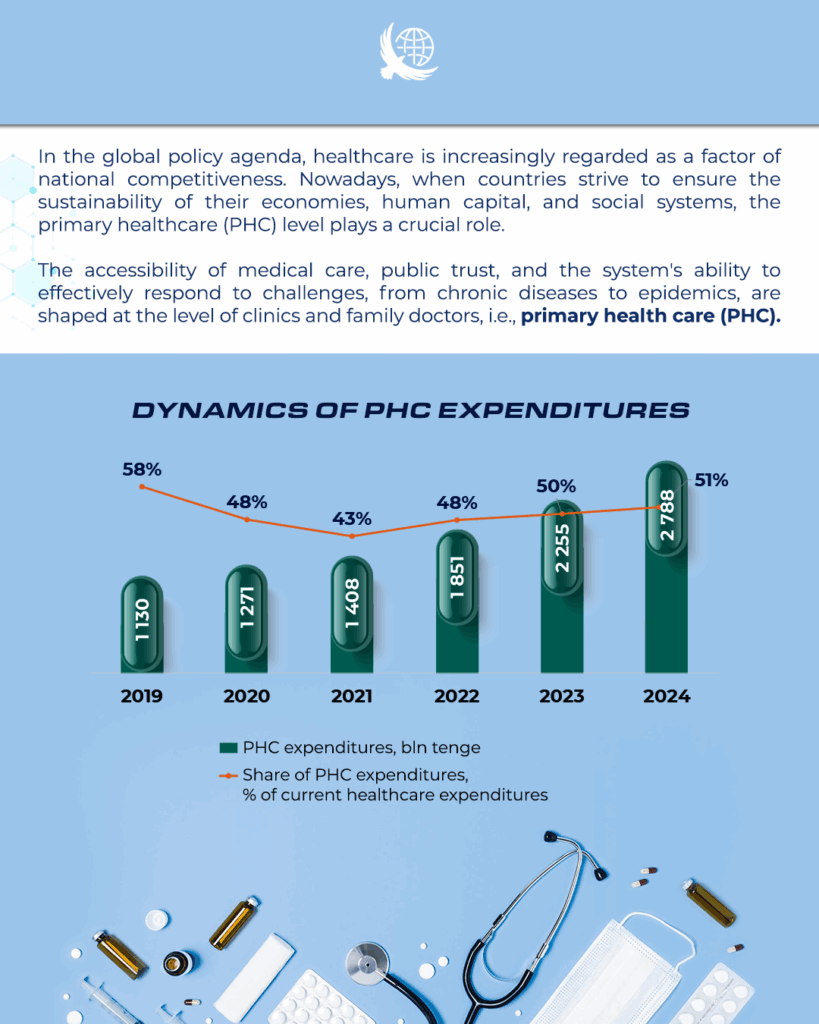
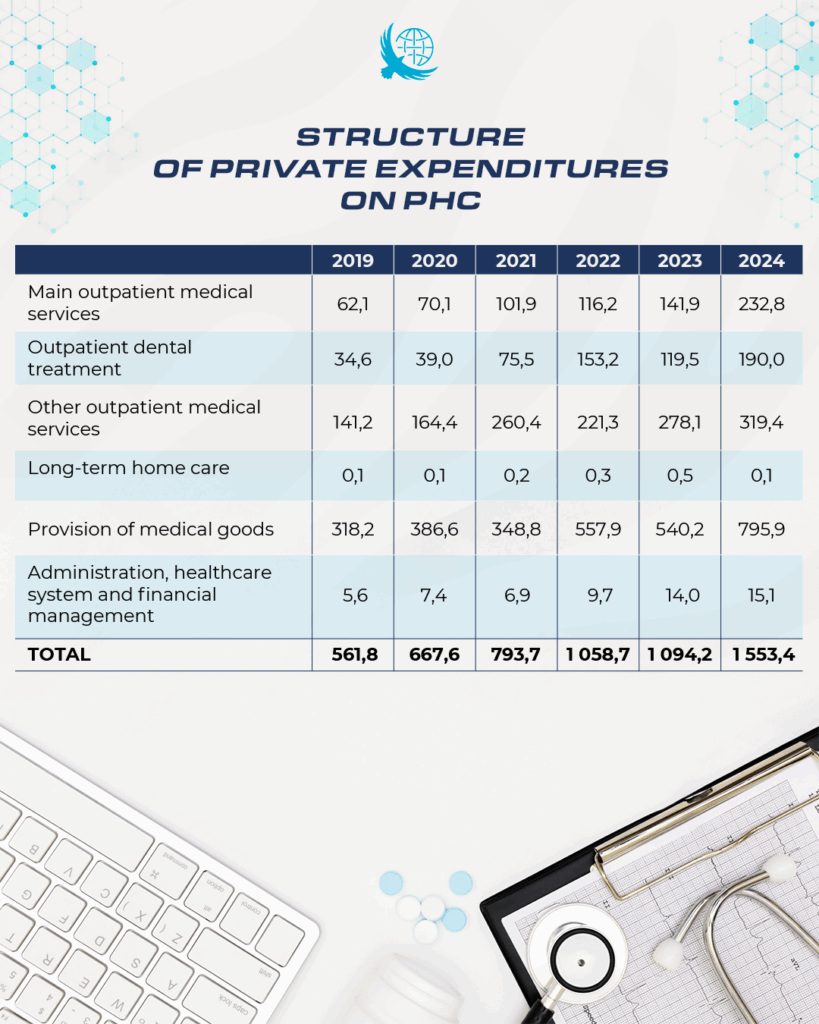
Kazakhstanis continue to pay considerably out of their own pockets, primarily for the purchase of medications (more than 50%). Total private spending on PHC in 2024 amounted to 1.55 trillion tenge, which is more than half of all spending on this level of care. This indicates low accessibility of PHC.
Preventive expenditures also remain relatively low. In 2019, preventive spending accounted for about 3.5% of total health expenditures in Kazakhstan, but by 2023 this figure had decreased to 2.1%.
In OECD countries, by contrast, preventive spending has been increasing, averaging 5%, and reaching 10-12% in countries such as the Netherlands, Austria, and the United Kingdom.
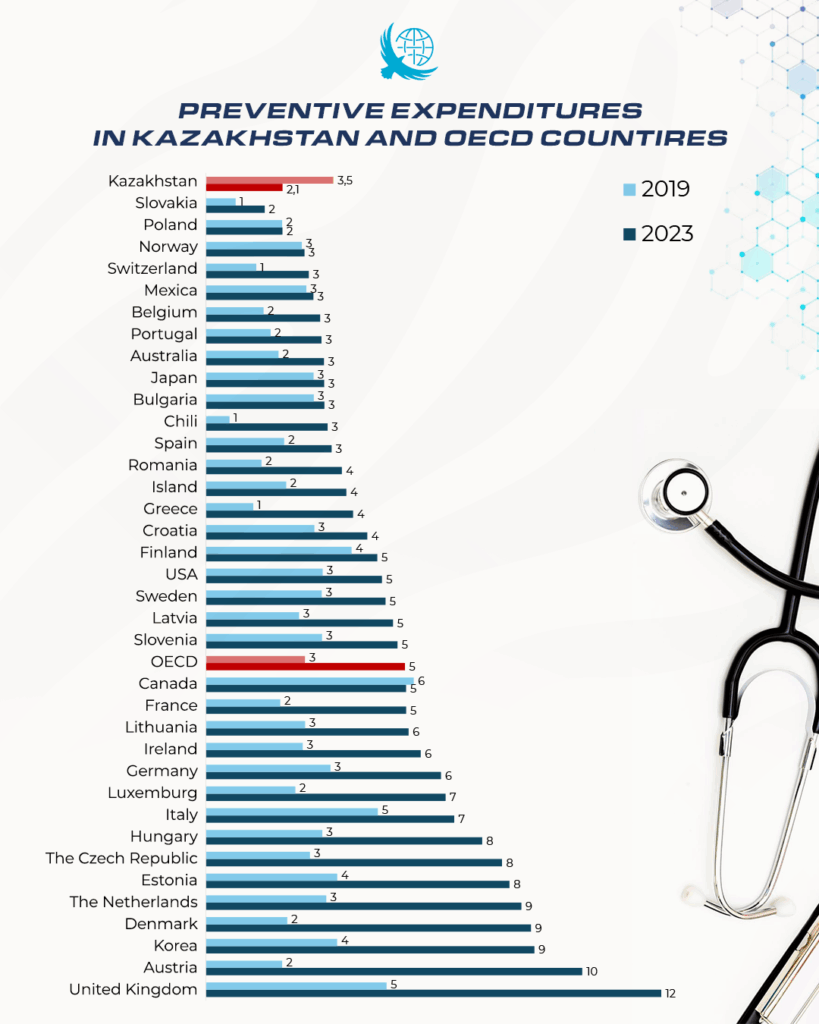
Thus, despite overall funding growth, a structural imbalance persists: the preventive component of PHC remains underfunded, while the financial burden is gradually shifting to the population. This highlights the need to revise priorities toward prevention and early intervention so that PHC truly becomes the foundation of a sustainable health system.
Effective PHC as A Strategic Tool for Cost Control and Improving the Sustainability of the Health System
Today, about 90% of medical cases can be effectively resolved at the PHC level, and this is precisely where the greatest return on every tenge invested is generated. The cost of care increases sharply when moving to specialized and inpatient services. Therefore, the priority lies not in simply increasing total healthcare spending but in rationally reallocating resources toward primary care. The more cases that can be addressed at the primary healthcare level through timely detection of diseases, high-quality care for chronic patients, effective prevention, and consultations, the less unnecessary hospital admissions, examinations, and costly interventions at higher levels will be required.
International experience confirms this approach: strengthening PHC reduces hospitalization rates, limits excessive prescriptions, and optimizes drug use. According to WHO and World Bank estimates, every dollar invested in PHC yields up to 10 dollars in economic benefit, and investments in vaccination yield up to 44 dollars. This means that financing primary health care is a way to reduce costs rather than increase them. It is a long-term investment that simultaneously improves the efficiency of the system, improves public health, and strengthens the country’s economic stability.
Along with the economic effect, a strong primary healthcare network has a direct impact on key population health indicators, contributes to reducing maternal and infant mortality, increases life expectancy, and builds human capital, which is the foundation of a country’s competitiveness.
To achieve this effect, the following systemic changes are necessary. Firstly, increasing the priority of primary care through a step-by-step increase in per capita standards, with due account for demographic, epidemiological, and regional factors. Funding should be based on the actual needs of the population, rather than historical limits. Secondly, revision of the expenditure structure is required, i.e., a gradual shift in emphasis from inpatient and high-tech care to prevention and comprehensive patient management at the primary care level, the introduction of pay-for-performance mechanisms, and the development of integrated doctor-nurse-social worker teams. And thirdly, strengthening the preventive function of primary care, expanding screening, improving the quality of care for patients with chronic diseases, and increasing the role of general practitioners and nurses in shaping healthy behavioral practices.
Thus, investing in PHC is a strategic choice in favor of a more effective, accessible, and sustainable healthcare system, where prevention and early intervention become the foundation of national health and economic stability.


